Autoclaves is a high-pressure vessel that uses pressure higher than atmospheric pressure to raise the boiling point of water above 100°C, allowing for the sterilization of liquids or instruments. It is an ideal device for use in laboratory and medical fields.
Application Scope
Vertical Autoclaves:
A vertical autoclaves is a fully automatic, high-temperature, high-pressure rapid sterilization device that uses pressurized steam as the sterilizing medium. It is designed for use in various medical, health, and biomedical research institutions, including disease control centers, inspection and quarantine agencies, hospital laboratories, and university biological research labs. This autoclave is capable of sterilizing non-sealed liquids, culture media, glass and metal instruments, as well as contaminated solid waste.
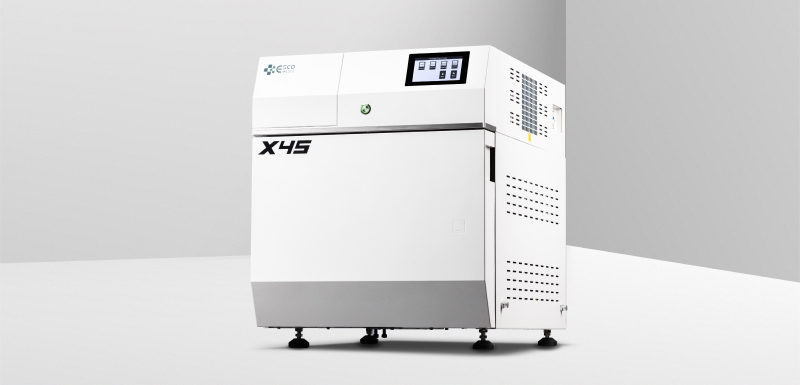
Pulsed Vacuum Sterilizer:
A pulsed vacuum sterilizer specifically sterilizes items that contain or may contain highly pathogenic microorganisms in high-level biosafety laboratories. It not only ensures the sterilization of the items but also guarantees the sterilized discharge of gases, vapors, and liquids during the sterilization process. This means that the sterilization process also sterilizes all gases, vapors, and liquids released during the cycle, ensuring a completely sterile environment throughout.
Correct usage method
Preliminary Treatment of Sterilized Items
Disinfect medical instruments, bed linens, clothing, and other items that have come into contact with pathogenic microorganisms using a chemical disinfectant, followed by routine cleaning. This is especially important for items used in infectious disease wards, where you must disinfect them strictly before cleaning. For regular cleaning, start by soaking and scrubbing the items in a detergent solution to remove grease, blood stains, and other contaminants, then rinse thoroughly with running water. Items with joints, teeth, grooves, or gaps should be opened or disassembled to allow for thorough cleaning. After washing, items should be dried and packaged according to clinical needs to prevent re-contamination. Containers and transport tools for contaminated items should be strictly separated and clearly marked to prevent cross-contamination.

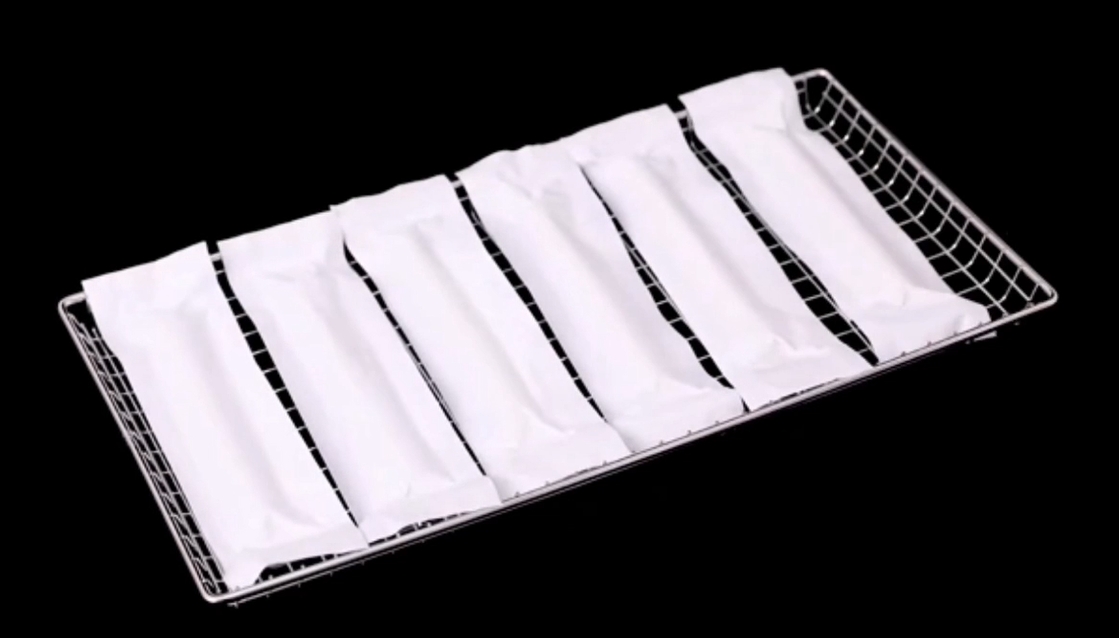
Packaging and Containers for Sterilized Items
The packaging of sterilized items should be appropriate. Use double-layer cloth packaging, with white cotton cloth. Wash new cloth to remove starch before use. Secure items with string to prevent loosening, but avoid tying them too tightly. When selecting containers for sterilization, choose those that can block external microorganisms while allowing good steam penetration. For example, specially designed sterilization boxes for syringes or storage tanks for dressings. Household aluminum containers are unsuitable because steam has difficulty penetrating them, and air cannot escape, often resulting in ineffective sterilization. Comparative tests have shown that their contamination rates are much higher than medical-grade aluminum boxes. Therefore, do not use household aluminum containers for sterilizing syringes or instruments.
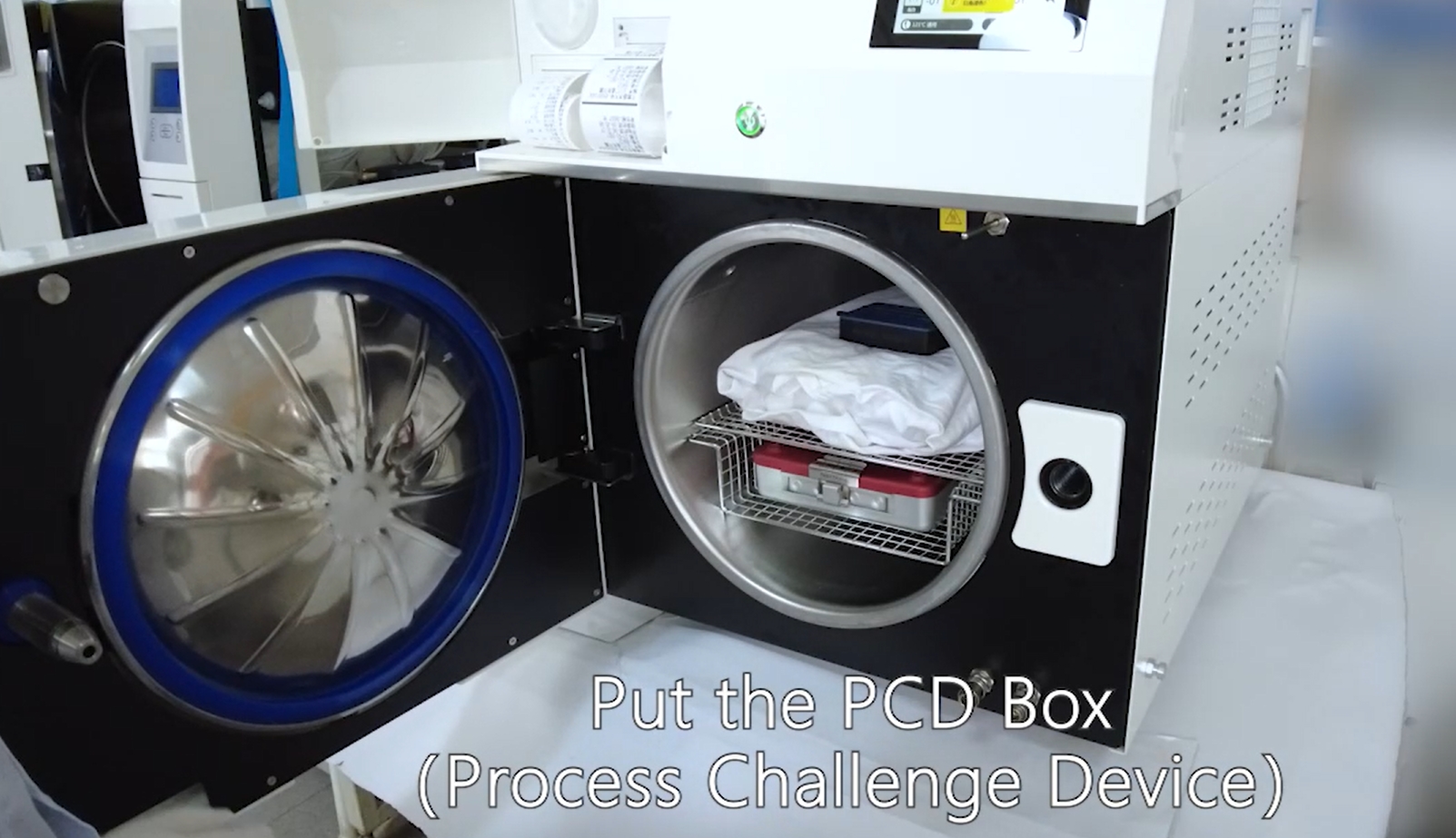
Proper Arrangement of Sterilized Items
Overloading or improper arrangement of items in the sterilization chamber can affect the sterilization process. Do not overcrowd items or exceed the chamber’s capacity. Whenever possible, place similar items together in one load. If you mix different types of items, base the sterilization conditions on the most difficult-to-sterilize item. Arrange items with gaps between them—horizontally, vertically, and laterally—to allow steam to penetrate easily. Place large sterilization packs upright on the top shelf, with smaller packages on the lower shelf. Also, place large enameled containers and storage tanks upright. When you sterilize fabric and metal items together, place metal items at the bottom to ensure even heating and prevent condensation from wetting the fabric packaging.
Reasonable Calculation of Sterilization Time
Sterilization time consists of:
Penetration time: The sterilization temperature reaches all areas of the load, starting in the chamber and extending to the most difficult-to-penetrate parts.
Holding time: The time required to kill microorganisms, typically measured by the time needed to kill Bacillus stearothermophilus spores.
Safety time: Extra time added to ensure the sterilization is complete and reliable. This typically represents half of the thermal death time, depending on the type of items you are sterilizing.Easily heat-conductive metal equipment requires no safety time. During the sterilization process, monitor the pressure gauge and adjust the air intake to maintain the correct pressure until the sterilization time is complete. If the pressure or temperature drops during sterilization, you should reheat and repressure the chamber and restart the timing.
Safety Precautions
Before each sterilization cycle, check that the sterilizer is in good working condition, especially the safety valve. Do not reduce the pressure too quickly after sterilization. Wait until the pressure gauge reads “0” before opening the chamber door. If the chamber contains bottled solutions, opening the door suddenly can cause the glass to crack due to thermal shock. Be cautious when opening the door too wide, as this may allow cold air to enter rapidly, causing condensation around the cloth packaging, blocking steam vents and making the items wet.