The promotion of oral medical reform and the popularization of oral health knowledge have enhanced people’s awareness of self-protection, making oral health an urgent problem in today’s society. Dental instruments are the basic tools for diagnosing and treating patients. A large number of studies have shown that dental devices are the vectors of healthcare-associated infections, and their modes of transmission include surface contamination, air pollution, internal contamination, and direct injury.
Most procedures performed by dental professionals occur within the mouth, which harbors a vast number of microorganisms. During treatment, instruments often come into contact with patients’ blood, saliva, and other bodily fluids. The risk level of dental instruments varies: high-risk tools include extraction forceps, scalers, endodontic files, and implant handpieces; moderate-risk instruments consist of mirrors, orthodontic pliers, and crown removers; while low-risk tools encompass carving knives and dental hammers. Currently, hospital-acquired infections are on the rise globally, prompting serious attention from healthcare administrators and clinicians.
Dental clinics must implement effective infection control protocols, much like guests expect their rooms and shared spaces in luxury hotels to be clean. Patients also desire standard infection control measures from their dentists. In response to the widespread lack of disinfection awareness in dental clinics, the Ministry of Health in China, after thorough research, established the “Technical Operating Standards for the Disinfection of Dental Treatment Instruments” in 2005, reinforcing the importance of instrument disinfection to ensure medical quality and safety.

01. The significance of sterilization and disinfection of oral instruments
There is a significant amount of literature reporting on bacterial and viral contamination in dental clinics, highlighting the mutual transmission of diseases between oral practitioners and patients. One major reason for cross-infection is the negligence of proper disinfection protocols for dental instruments.
- Controlling Infection Spread: Dental clinics are hotspots for pathogenic microorganisms. Microbes from dental patients and carriers can be expelled in various forms, contaminating the surrounding environment. There are numerous ways infections can spread within dental clinics. For instance, inadequately disinfected oral instruments, blood and saliva carrying the hepatitis B virus, aerosols laden with viruses, dust from dental calculus, and droplets from coughing can all serve as vectors for hepatitis B transmission if not promptly neutralized. This can lead to infections in the clinic, posing a threat to other patients, accompanying persons, and even dental staff. A notable example is the first reported case of an AIDS patient in Liaoning Province, who contracted the virus during a dental procedure while working in Africa
- Encouraging Patient Visits: Traditionally, many dental clinics have overlooked sterilization and disinfection, leaving serious gaps in safety. A significant reason patients hesitate to visit dental clinics is the fear of contamination and disinfection issues. This underscores the need for clinics to prioritize instrument sterilization and to actively communicate with patients about these measures.
- Enhancing Healthcare Quality: Preventing cross-infection in dental clinics is not just a matter of occupational health for oral practitioners and staff; it is crucial for enhancing healthcare quality. Without a strong focus on sterilization and disinfection, dental clinics risk becoming venues for transmitting infections between practitioners and patients. There is an increasing awareness that the dental treatment process is a critical pathway for infections, necessitating the implementation of appropriate control measures. Dental care providers and those responsible for instrument disinfection should master infection prevention and control, adhere to standard precautions, and strictly follow relevant regulations.

02. Principles of sterilization and disinfection of oral instruments
All practitioners must sterilize oral treatment instruments that contact patients’ wounds, blood, or damaged mucous membranes.Instruments that enter sterile tissues also require sterilization before use. This includes dental handpieces, burs, endodontic instruments, extraction instruments, surgical instruments, periodontal treatment instruments, and dressings. Instruments that contact intact mucous membranes or skin must be disinfected. This includes mouth mirrors, probes, and dental tweezers. They must be disinfected before use. This includes various physical measuring devices, impression trays, and rinsing cups used for auxiliary treatment. Items that contact patients’ bodily fluids or blood must be disinfected. This includes restorative and orthodontic models. Practitioners must disinfect them before sending them to the technician’s room for processing.
03. Characteristics of sterilization and disinfection of oral instruments
-
Variety of Oral Instruments
Dental clinics have a wide variety of oral instruments. These include dental handpieces, teeth cleaning tools, examination instruments, impression trays, gypsum models, dentures, X-ray films, syringes, needles, extraction tools, filling instruments, periodontal surgical instruments, and various dental drills. All these instruments should be used only after reliable disinfection.
-
Special Disinfection of Dental Handpieces
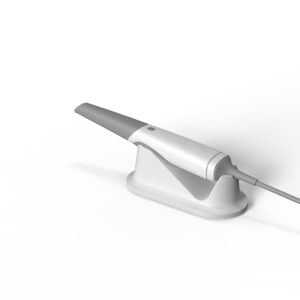
Dental professionals commonly use dental handpieces in clinical oral treatment. Because these instruments are in close contact with the patient’s saliva, blood, gingival crevicular fluid, and dental plaque during treatment, practitioners must disinfect the surface and internal turbine components and pipelines of the handpiece after use. Additionally, when the pneumatic turbine handpiece is in operation, it can draw in surrounding air into the airflow. When the operation stops, the system suddenly cuts off the high-pressure input air, causing the handpiece to gradually slow down and stop. Consequently, this leads to more surrounding air being drawn into the depressurized pipeline system. Therefore, practitioners must disinfect each handpiece for individual use.
-
Frequent Sterilization and Disinfection
The sterilization and disinfection of dental instruments often occur in clinical practice, requiring rapid and reliable disinfection. Dental phones, for example, are delicate instruments, fragile and expensive; Clinics can’t afford to buy a lot of phones. Therefore, the disinfection process must be as fast as possible to avoid damaging the instruments. Too long disinfection time will cause certain damage to the equipment.
04. Methods for Sterilization and Disinfection of Oral Instruments
Disinfection in dental clinics is a crucial measure for preventing infections and the spread of infectious diseases. In recent years, with the rapid development of medicine, the methods of disinfection in dental clinics have become increasingly diverse, with a rapid improvement in disinfection standards moving towards standardization and legalization. Sterilization refers to the process of eliminating various microorganisms from instruments or environmental surfaces, including the destruction of highly resistant bacterial spores. Disinfection, on the other hand, involves the destruction of pathogenic microorganisms but does not necessarily affect all microorganisms.

Generally, we hope that sterilization and disinfection agents can achieve the following effects:
- Effective against all microorganisms,
- Non-corrosive and safe to use,
- No residues,
- Sterile—ensuring no contamination before and during use,
- Quick action,
- Good chemical compatibility,
- Good material compatibility,
- Economical (considering price, preparation time, usage time, personal protection, and waste).